Major Advance in Intestinal Health

Probiotics are emerging as enormously popular health supplements.
When one ingests a probiotic, they add bacteria to their digestive tract that produce benefits ranging from alleviating intestinal distress to strengthening immunity.
Another virtue of probiotics is that they can slowly crowd out harmful bacteria strains in the intestines.
In a significant advance, a natural method of selectively killing undesirable bacteria has been developed.
When combined with a probiotic in the animal model, there was an exponential increase in beneficial bacteria with a parallel decrease in unfriendly flora like E. coli.1-3
This article describes a novel way of optimizing probiotic efficacy.
Most people in the United States have likely never heard of phage therapy. It was discovered in pre-World War I Eastern Europe, and for much of the pre-World War II era, it was thought to be a promising approach to controlling bacterial illnesses.4-6
In the 1940s, industrial giants like Eli Lily and L’Oréal developed bacteriophage “cocktails” aimed at treating a variety of bacterial infections. But the advent of antibiotics quickly cost phages the spotlight, though their effectiveness has never been in question.7
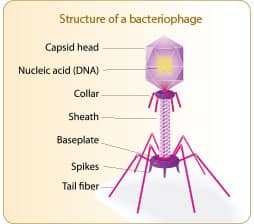
Phage therapy uses bacteriophages, which are submicroscopic packages of DNA or RNA enclosed in a protein envelope that selectively target harmful bacteria.
The name bacteriophage literally means “bacteria eating.” A bacteriophage attaches itself to a bacterial cell wall and then destroys the host bacteria.
Bacteriophages are ubiquitous in nature, meaning they can be found almost everywhere—from soil, hot springs and the ocean depths to the animal and human body.8
The name bacteriophage literally means “bacteria eating.”
Phages are a common and important component of gut flora and are found in various other parts of the human body such as the mouth and skin.8,9 Phages are currently used in the food industry to control disease-causing organisms.10-12
Numerous phages are classed as GRAS—or “generally recognized as safe”—and are commonly used for a variety of different applications, from controlling Listeria in cheese and E. coli in meat and on food-contact surfaces, to Salmonella in food.
With the targeted use of bacteriophages, it is possible to seek out and effectively reduce specific populations of unhealthy organisms that have taken over the intestinal microbiome.
The use of bacteriophages allows an exceptionally specific approach to eliminating detrimental bacteria. This is in direct contrast to antibiotics, which employ a mass-killing technique that eliminates healthy and detrimental bacteria, leaving us vulnerable to attack by other organisms.13
By removing common pathogenic bacteria in one’s gut, bacteriophages enable beneficial probiotic bacteria to thrive, allowing them to more effectively rebalance the microbiome.
When phages are combined with probiotics in animal models there are huge reductions in the targeted harmful bacteria with a simultaneous increase in beneficial bacteria.
The Importance of a Healthy Gut
When scientists speak of the intestinal microbiome, they refer to the community of trillions of microorganisms that populate the human gut.14We’re just now beginning to understand that this collection of microorganisms can determine our state of health and illness.
It is impossible to avoid all threats to our intestinal microbiome. The increase in our consumption of meats, fats, processed carbohydrates, preservatives, and other additives can alter our bacterial populations.15-17 And, of course, the overuse of antibiotics kills both healthy and bad bacteria indiscriminately.7,18,19 As a result, our delicate microbiome is becoming disrupted and imbalanced, which results in a condition called dysbiosis.
Dysbiosis is associated with almost every known disease process, from obesity and cancer to cardiovascular disease, diabetes, allergic reactions, neurodegenerative disorders such as Alzheimer’s, and even mental health issues such as depression.20-22
Imbalances in the intestinal microbiome steadily worsen with age,23-26 and can be blamed for such common complaints as feeling generally unwell, reduced sleep quality, and feeling “foggy.”27-31
The impact of an unbalanced microbiome can also lead to another disorder related to dysbiosis called small intestinal bacterial overgrowth. People with this condition often have vague but persistent abdominal symptoms, such as pain, bloating, indigestion, gas, or cramping.32,33 And in older adults, small intestinal bacterial overgrowth can contribute to malnutrition and eventual frailty, making the condition a major threat to the elderly.32,34
Giving Probiotics a Boost
Many people live in a state of dysbiosis or imbalance that not only threatens their long-term health, but may also contribute to sleep disorders, to a sense of malaise or “fogginess,” and to a range of stomach distress issues that cannot be explained by a specific disease. Fortunately, many studies have shown that positively changing the microbiome—shifting it toward a healthy profile and away from dysbiosis—can also change symptoms and disease risk.14,35,36
One important way of improving the intestinal microbiome is through the use of probiotic bacteria. Probiotics are a great additive therapy that increase the abundance of organisms that can rebalance an ailing microbiome. In some cases, however, probiotics by themselves have difficulty competing with the more aggressive microbes that contribute to dysbiosis in the first place.
A more comprehensive approach is to use probiotics in combination with another therapy, one that selectively targets and reduces the troublesome bacteria that are taking over the microbiome. This approach of targeting harmful bacteria while replenishing beneficial bacteria can make way for probiotics to better help restore the microbiome to a healthy, balanced state. That is how phage therapy works.
Phage therapy reduces potentially troublesome organisms that are overabundant in the microbiome, allowing beneficial organisms to flourish. This helps restore the microbiome to a healthy, balanced state.37
WHAT YOU NEED TO KNOW
 |
The Revival of Phage Therapy
- An imbalance in the intestinal microbiome (dysbiosis) is now associated with many serious age-related disorders. Studies show that it is prevalent in older people, particularly those with sleep disorders, vague abdominal complaints, and malaise.
- Changing the intestinal microbiome towards a state of improved health and function is a desirable solution, but until now options have been limited.
- Bacteriophages selectively target and destroy specific harmful bacteria.
- In combination with a mixture of probiotic bacteria, a cocktail of bacteriophages has been shown to reduce the abundance of undesirable bacteria, while freeing beneficial organisms to thrive and increase in numbers.
- Using this probiotic/bacteriophage mixture shows high promise in relieving the functional changes and tissue damage wrought by dysbiosis, and should be added to the regimen of anyone interested in rebalancing their microbiomes to feel better.
Combating E. coli Bacteria
Escherichia coli (E. coli) is a bacterium that normally lives in our intestines. Most types of E. coli are harmless, but some can cause disease.
A troublesome strain of E. coli called H10407 causes abdominal cramps, diarrhea, and gas.38,39 This pathologic E. coli strain also suppresses growth of beneficial bacteria and produces a state of dysbiosis.40
In an effort to help restore a balanced and healthy microbiome, researchers have developed a cocktail of bacteriophages that target dangerous strains of E. coli.
Unlike typical pre- or probiotics, this phage cocktail is effective within hours, not days, and in very small doses.40 It functions not only in the colon (large intestine), where dysbiosis is a problem, but also in the small intestine, where undesirable bacterial overgrowth occurs. It does not cause flatulence, a constant problem with fiber-containing prebiotics.40
Laboratory studies show that this form of phage therapy removes harmful bacteria, making way for beneficial probiotic bacteria to establish and form a healthy microbiome. This has been demonstrated—with impressive results.
Phage Cocktail Promotes Survival of Probiotic Organisms
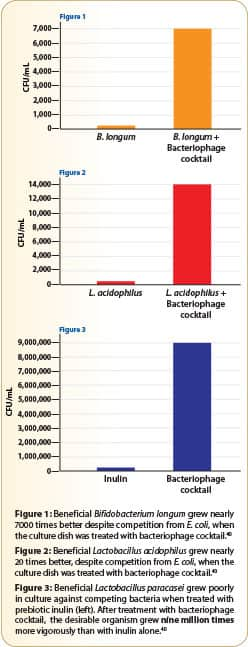
In one experiment, culture dishes were prepared with a beneficial bacteria (Bifidobacterium longum), along with a competitive E. coli bacteria.40
A second set of dishes was prepared to which the bacteriophage mixture was added. After just 5 hours, there was a visible difference.
In the dishes without bacteriophage, there was little growth of the desirable B. longum organisms, indicating their inability to compete with E. coli.
In the dishes with the bacteriophages, colonies of B. longum skyrocketed to more than 7,000 times their numbers compared to dishes without the bacteriophage. This study demonstrates that the competitive E. coli had been greatly removed from the picture by the bacteriophage (Figure 1).
In a related experiment, a probiotic organism (Lactobacillus acidophilus) was grown in culture, again in competition with E. coli.40 In a very similar fashion, without the phage cocktail, the E. coli suppressed growth of the beneficial L. acidophilus. However, in the presence of the phage mixture, L. acidophilus thrived, reaching colony counts that were 20-fold higher compared to the culture not receiving the phages. (Figure 2). In similar experiments, growth of the probiotic organism L. rhamnosus was enhanced 15-fold and the beneficial B. bifidum was enhanced nearly 10-fold when grown in culture with the phage cocktail.
These experiments demonstrate the value of the phage mixture in promoting the growth and survival of probiotic organisms.
In another Petri dish experiment, the common prebiotic inulin was used in an attempt to stimulate the growth of the beneficial probiotic Lactobacillus paracasei. When the prebiotic was used alone, it failed to ensure the survival of the desired organisms. But when the phage mixture was added, it produced an astonishing nine million-fold increase in growth of the probiotic Lactobacillus paracasei (Figure 3).
Phage Cocktail Decreases E. coli and Improves Normal Gastrointestinal Function
Moving out of the Petri dish and into the animal model, one group of laboratory mice was given the probiotic B. longum in combination with the disease-causing E. coli strain H10407.41 A second group of mice was given the same mixture, but with the addition of the phage cocktail that targets E. coli.
After 24 hours, compared with the control group, animals in the phage-treated group gave powerful evidence of a reduction in the disease-causing bacteria as can be seen on the following page:
- About a 10-fold decrease of E. coli in the small intestine
- About a 100-fold decrease of E. coli in the colon (large intestine)
- About a 100-fold decrease of E. coli in fecal matter
At the same time, the phage-treated animals showed remarkable increases in the beneficial (B. longum) bacteria as follows:
- About 100-fold increase of B. longum in the small intestine
- About 100-fold increase of B. longum in the colon
- About 40-fold increase of B. longum in fecal matter
This study also revealed marked differences in the appearance of tissue samples and digestive function across the different groups of mice.
Mice treated with E. coli and B. longum alone were constipated, and intestinal segments showed swelling, redness, and leaks compared with healthy animals. The mice given B. longum and E. coli plus the phage mixture had normal bowel movements, while their intestinal tissues showed no detrimental changes.
Safety of Phage Therapy

In 1981, Russian researchers reported the successful use of phage therapy to treat antibiotic-associated dysbiosis—displacement of normal intestinal bacteria with pathogenic bacteria—in 500 low-birth-weight infants.
The subjects had all been given antibiotics for at least two to three weeks to treat sepsis and pneumonia, killing off their gut bacteria. They were then administered both a specific bacteriophage and a probiotic (Bifidobacteria) strain. The infants experienced both depletion of their pathogenic bacteria and replenishment of healthy, intestinal bacteria.42
Phage therapy has been used for a wide variety of infections involving numerous pathogens. Therapies have included infections of the gastrointestinal tract, skin, head and neck, bone, chest, and abdomen—and have involved an array of pathogens such as Staphylococcus, Streptococcus, E. coli, Salmonella, and Pseudomonas. Success rates range up to 80%-95% for phage therapy with either no, or only mild reversible, side effects.5,42,43
Bacteriophages were successfully used in numerous human clinical and therapeutic settings and demonstrated an extremely strong safety profile.43-46
The reason for the very safe interaction between phages and human tissue likely results from human exposure to vast numbers of phages over the entire course of evolution. This naturally high human tolerance to phages contrasts sharply with the risks inherent in compounds that are relatively novel in human evolution—such as drugs.5
HOW “PHAGES” DIFFER FROM ANTIBIOTICS
 |
Antibiotics are considered one of the 20th century’s greatest scientific achievements.
But decades of widespread antibiotic use has created “superbugs” that are not easily killed by current pharmaceuticals. Many believe we have reached the end of the “antibiotic era.”
In severe cases, physicians desperately search for alternatives to save their patients’ lives.
This has prompted excitement about an innovative approach developed more than 100 years ago, but overlooked with the advent of antibiotics.
In fact, long before antibiotics were discovered, Eastern European doctors were successfully neutralizing bacterial infections with phage therapy, a treatment aimed at selectively targeting and destroying harmful bacteria.
With the rise in antibiotic-resistant bacteria, phage therapy is experiencing a revival among the scientific community because of its effectiveness and safety profile. The potential for phage therapy is so great that just last year the National Institutes of Health sponsored a symposium titled:
"Bacteriophage Therapy: An Alternative Strategy to Combat Drug Resistance"
Phage cocktails have been shown to effectively treat common bacterial invaders, including staph, strep, and E. coli.1-3
Phage therapy also beneficially encourages growth of healthy bacteria in the gut microbiome, which can also reduce harmful bacteria.
With so much scientific investigation into the multiple health benefits of a balanced microbiome, phage therapy is rapidly emerging as a new venue to enhance the benefits of probiotics.
Summary
In addition to being associated with major age-related disorders, an unbalanced intestinal microbiome (dysbiosis) can also be responsible for general “blah” feelings as well as vague but troubling intestinal symptoms that plague aging individuals.
A novel approach to bringing the gut microbiome back into a healthy balance uses safe bacteriophages to selectively reduce harmful bacteria while encouraging beneficial probiotic organisms to flourish.
Called phage therapy, this technique is harmless to humans, but deadly for specific, troublesome bacteria.
Studies show that when probiotic organisms are accompanied by targeted phage therapy, the beneficial bacteria grow up to thousands of times their baseline rate, thanks to the removal of the more aggressive microbes.
Phage therapy shows real promise in relieving the functional changes and tissue damage wrought by dysbiosis and could be especially valuable for aging individuals experiencing intestinal discomfort, sleep disturbances, or general malaise.
By Sonia Whitman
Article extracted from Life Extension Magazine


Social Login